Welcome to the Day in the life of being a resident at North Shore-LIJ Neurology at Northwell!
We hope that this page can provide insight into how our residents thrive together as a community. We are happy to walk you through the day-to-day of being a neurology resident at our program. As you may already know, our residency program encompasses two hospitals: North Shore University Hospital and Long Island Jewish Hospital. The split between the two hospitals is roughly ~70% NSUH and ~30% LIJ.
- At North Shore University Hospital, our residents rotate primarily through three different services: Consult, floors/EMU and Stroke.
- At LIJ Medical Center, residents rotate on the stroke team as well as the consult team.


Formal Didactics: Morning didactics occur every day. These take the form of either morning report in which the night-float resident presents a case to the group, a resident-directed case conference geared towards practical aspects of inpatient epilepsy, neuro-vascular conference, or grand rounds.
Noontime didactics occur every day. These take the form of traditional lectures led by faculty members, board-review sessions led by senior residents, Chairman Rounds, or Continuum article reviews.
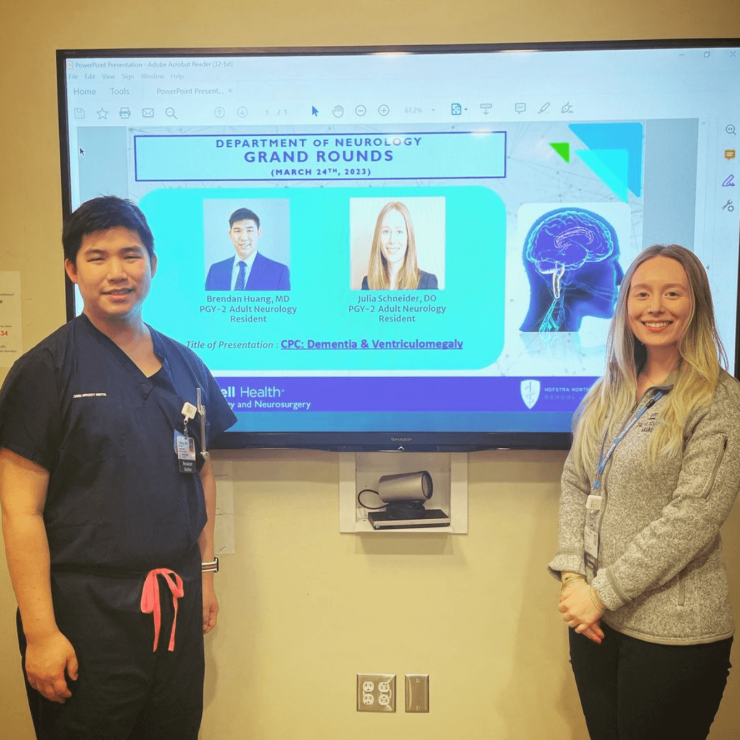
Medical Education Opportunities: Throughout residency, there are a myriad of opportunities to teach the next generation. Even as a PGY2 resident, you will teach MS3 and MS4 medical students and other rotators who are part of each of the inpatient teams. As a PGY3, you begin to oversee the team as a “senior resident” and help guide PGY2 residents while on night-float rotations. PGY4s help oversee medical education for the residency as a whole and each take turns as “Education Chief”, ensuring that a broad range of board-style content is covered. For PGY3s and PGY4s who are interested in medical education, an “Education Track” is available.

